Overall Response Rate and solid tumors – the magic number… to date
When we design clinical trials, we want to show clinically meaningful improvements for patients, measured by endpoints that are relevant for their specific disease.
In cancer clinical trials, the gold standard demonstration of efficacy is overall survival (OS). However, developing a new medicine – beginning with early phase testing and continuing all the way to a pivotal Phase 3 trial with an OS endpoint and ultimate regulatory approval – can take several years – years many patients do not have.
The oncology field relies on various ‘surrogate’ endpoints – such as progression-free survival (PFS), disease-free survival (DFS) and overall response rate (ORR) – to identify signs of treatment benefit earlier than when overall survival data would have matured. Since the 1970’s, when cancer treatments consisted primarily of chemotherapy and radiation, physicians in clinical trials have assessed treatment responses by measuring the physical size of a tumor.1 Today, this is typically done via radiographic assessment of the longest side of selected tumor lesions in key anatomic locations. The change in size is evaluated using the RECIST (Response Evaluation Criteria In Solid Tumors) criteria:
- Complete Response (CR) – Measured tumors have completely disappeared.
- Partial Response (PR) – Measured tumors have decreased in size by 30% or more.
- Stable Disease (SD) – Measured tumors have either decreased by up to 29% or grown by less than 20%.
- Progressive Disease (PD) – Measured tumors have grown by 20% or more.
RECIST is the most common response criteria used in early phases of drug development to evaluate if new investigational treatments are working and whether it makes sense to advance them to late-stage development, with the ultimate aim to seek marketing authorisation from global health authorities.
The overall response rate, which is the proportion of patients achieving complete or partial responses, has traditionally been the ’magic number’ that serves as a surrogate of OS.
But with the rise of immune-based therapies for cancer – which can tend towards stabilizing a tumor without large reductions in size – the limitations of RECIST-based evaluation are becoming more important.
The discussion concerning RECIST’s applicability to contemporary immuno-oncology is not entirely new. The question was raised as long as two decades ago, in a Journal of Clinical Oncology article by Ratain and Eckhardt:
“In the past, it was easy to prioritize agents for phase III trials based on their ability to induce objective tumor regression. However, a drug may be active without consistent achievement of high-level tumor regression…”
The authors go on to discuss the “subtle” effects of emerging agents such as early tyrosine kinase inhibitors, acknowledging the need “to be more flexible in our end points and our definitions of antitumor activity”.2
In a 2013 article in Clinical Cancer Research, the authors wrote: “Traditional RECIST are of limited use in clinical trials assessing immunotherapeutic agents.” They described four distinct response patterns observed among patients with advanced metastatic melanoma treated with an IO agent known as anti-CTLA-4 (Cytotoxic T-lymphocyte associated protein 4) therapy: shrinkage in baseline lesions without new lesions; durable stable disease; response after an initial increase in the total tumor burden; and a response in the presence of new lesions. Each of these patterns was associated with favorable survival, despite the third and fourth fitting the criteria for PD, a RECIST category historically associated with lack of clinical benefit.1
More recently, two articles pointed out the limitations of ORR including “a low correlation with OS in 91% of trials” as well as the promise of measuring “on-treatment changes in the amount or proportion of circulating tumor DNA in peripheral blood” to help identify patients who are benefiting from treatment “at earlier time points.” 3,4
Disease control rate: a stable choice?
In our investigations of a new generation of immunotherapies – by harnessing the power of the immune system using the T cell receptor (TCR) – we have determined that disease control rate (DCR) can be a more accurate predictor of clinical benefit than ORR.
DCR (which can also be referred to as clinical benefit rate or CBR) is defined as the percentage of patients with advanced or metastatic cancer who have achieved complete response (CR), partial response (PR) or stable disease (SD) after treatment in a clinical trial. The key is that it considers the potential for a patient to live longer because their tumor’s growth is slowed, not only if it is reversed.
The DCR approach to measurement was first introduced in 2008 by the Southwest Oncology Group5, when the team there showed that it was a stronger predictor of survival than response alone in advanced non-small cell lung cancer, and that this determination might be assessable early on during therapy. This is similar to what we saw in the registrational trial of the world’s first TCR therapy, and in multiple indications across our oncology pipeline.
Our ImmTAC (Immune Mobilizing Monoclonal T cell receptors Against Cancer) therapies have a mode of action that is distinct from most other immunotherapies – including antibodies and checkpoint inhibitors.
When we look at the data we have presented to date with our approved and most advanced investigational ImmTAC therapies, we see a clear story emerge: in order to measure the full extent of their clinical benefit – especially early on in treatment – as well as the durability of this benefit, we see that ORR underestimates and that DCR might be a more accurate tool.
Most notably, we observed in Phase 2 and Phase 3 trials in different forms of melanoma that the durability of clinical benefit (as measured by ctDNA molecular response, durability of tumor reduction and overall survival) was the same in patients with stable disease and mild tumor reduction as it was in patients with a partial or complete response.6,7,8
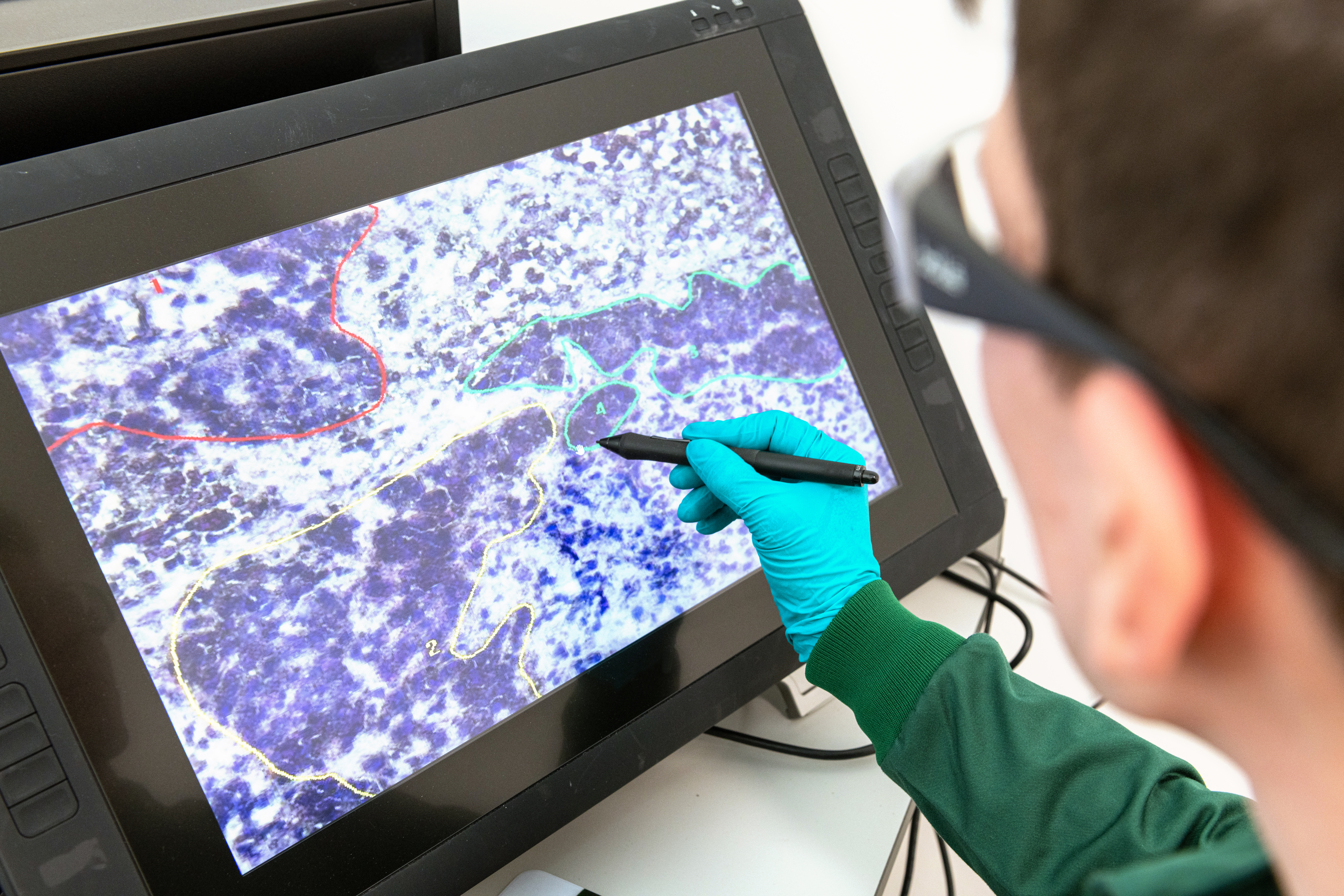
Further supporting the case for DCR, and as shown with other types of immunotherapy, we have reported cases of patients who experienced durable clinical benefits, despite initial growth of the tumor. This could be explained by the necrosis and inflammation of the lesion potentially representing pseudo progression of the tumor.
There is a need for more data to confirm the role of DCR in the early identification of clinical benefit, but the story is becoming clearer as we continue to analyze data generated from our clinical trials and presenting the insights at global oncology congresses.
What matters to patients is being able to live longer lives – emerging immunotherapies may allow them to do so. As the technology behind new cancer treatments evolves, so should the ways we measure their clinical benefit.
1The Clinical Viewpoint: Definitions, Limitations of RECIST, Practical Considerations of Measurement, Clin Cancer Res. 2013 May 15; 19(10): 2629–2636.
2https://ascopubs.org/doi/10.1200/JCO.2004.07.960
3ctDNA-Response evaluation criteria in solid tumors-a new measure in medical oncology, Jakobsen AKM et al. EJC 2023; 180:180-183
4Plasma ctDNA as a treatment response biomarker in metastatic cancers: evaluation by the RECIST working group, Wyatt AW et al. CCR 2024: 30(22): 5034-5041.
5Lara PN, et al. J Clin Oncol 2008;26:463-467.
6Hamid O L. Journal for ImmunoTherapy of Cancer 2023;11:e006747. doi:10.1136/jitc-2023-006747
7Ikeguchi A. Phase 3 KIMMTRAK trial IMCgp 100-202. ASCO 2024. Poster #9529.
8OS survival benefit with tebentafusp in mUM. N Engl J Med. 2021 Sep 23;385(13):1196-1206. doi: 10.1056/NEJMoa2103485
CM-GL--2500021
DOP: August 2025