HLA and ImmTAX technology
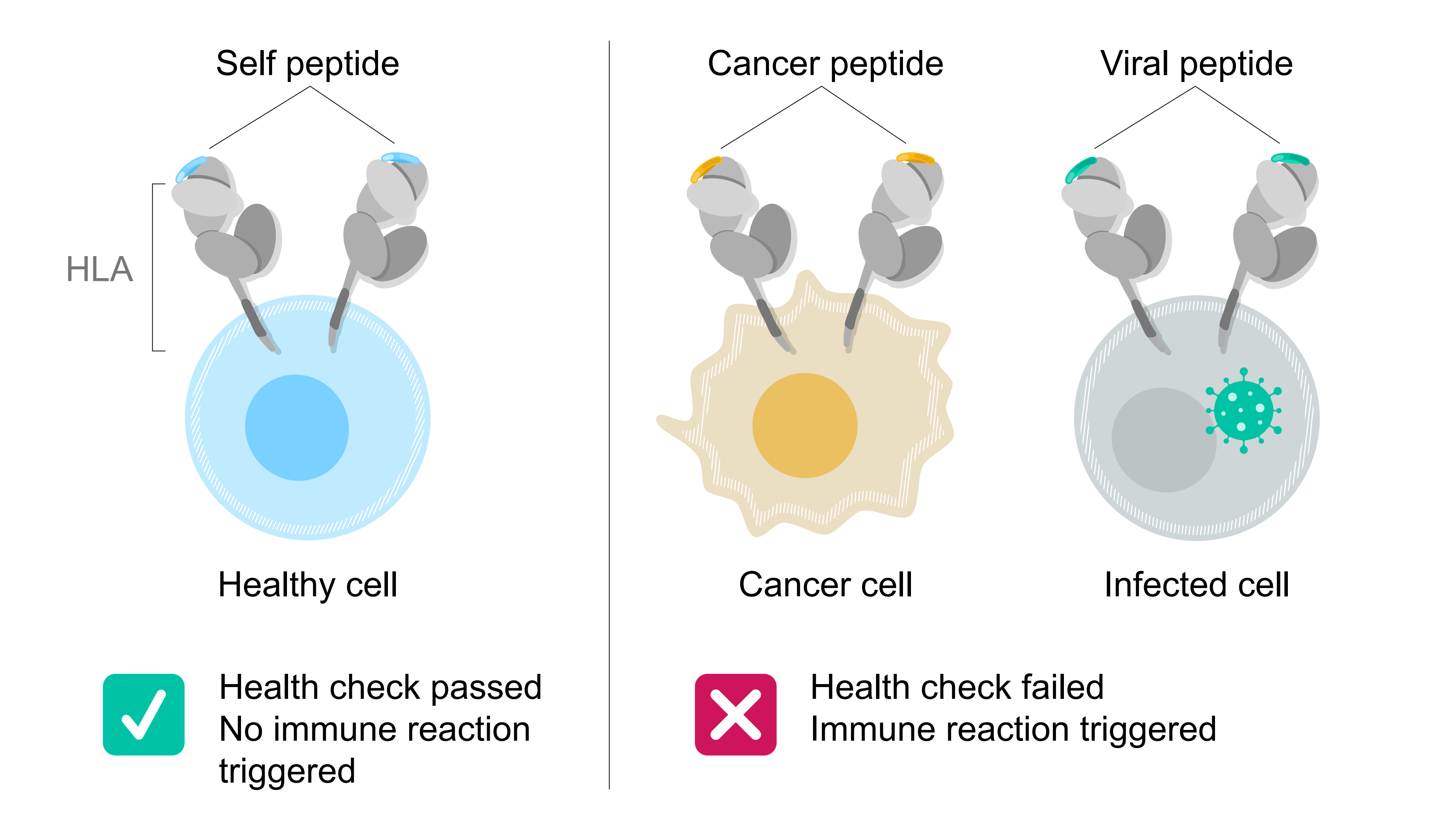
Much like the natural immune system, our ImmTAX technology is designed to recognize HLA markers and then send a signal to the body’s T cells to either activate them or turn them off.
An ImmTAX molecule does this by binding to the cell it wants to kill or protect – via the HLA system – and forming a bridge to the body’s T cells.
In cancer and infectious diseases, this bypasses the need for the person’s T cells to locate the unhealthy or infected cell on their own.2,3 In autoimmune diseases, it allows an inhibitory signal to be sent to T cells to stop them from wrongly attacking an otherwise healthy cell.4
Because the HLA system presents peptides from the vast majority (approximately 90%) of proteins made by the human body, ImmTAX molecules have the potential to fight a wide range of conditions, from cancers to infectious diseases and chronic autoimmune conditions.5